Journal
Stem Cell for Knee Pain
2024-03-15
More
For those looking for a promising treatment for arthritis and knee discomfort in Korea, stem cell treatment in Korea presents a viable option. This article will help you learn more about the advantages, possible side effects, and range of stem cell treatment alternatives that might be essential for anyone hoping to enhance joint health and mobility. We will help you to make an educated decision by learning more about this novel treatment to see if it's the best option for your knee-related problems.
Osteoarthritis
With millions of cases globally, osteoarthritis is among the most prevalent kind of arthritis. It arises from the gradual loss of the cushioning cartilage at the leading edges of the bones. As osteoarthritis may damage any joint, it typically affects the hands, knees, hips, and spine joints.
The majority of people with knee osteoarthritis are over 50, and women are more likely than males to get the disorder because of both musculoskeletal and hormonal causes. Nonetheless, there is a growing trend of younger individuals being affected by this condition, which puts them at risk for knee osteoarthritis that develops early.
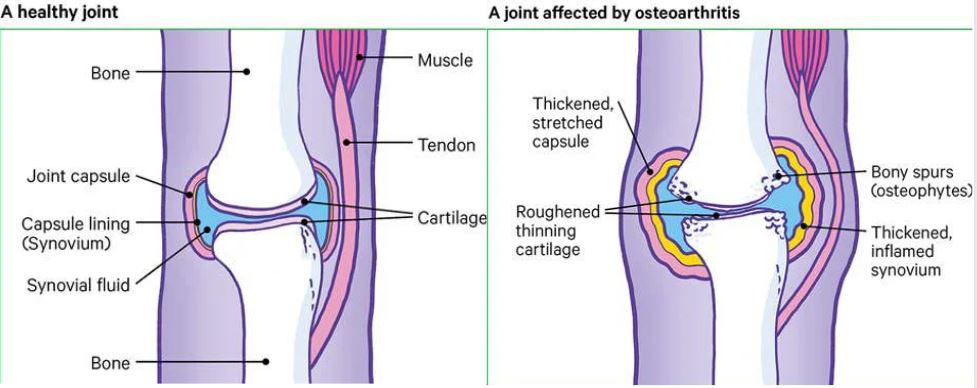
The most prevalent type of arthritis, osteoarthritis (OA), is brought on by age. A persistent condition called osteoarthritis leads to the degeneration of joint cartilage. While the exact origin of osteoarthritis varies from person to person, hormonal, genetic, chemically based, and mechanical variables are known to contribute to the condition's development. Osteoarthritis is characterized by joint discomfort and swelling, restricted movement, and a loss of flexibility. Damage to the cartilage, which typically covers the bones and absorbs stress to allow for smooth movement, is the cause of the disorder. The afflicted joint's cartilage gets worn down and roughened. As the condition worsens, the cartilage totally wears away, causing the bones to rub against one another.
Everybody's joints naturally degenerate and then repair over the course of a lifetime, however occasionally the body's healing process might result in structural or morphological abnormalities in our joints. Osteoarthritis is the term for these alterations that occur in one or more of your joints.
A joint is a location on one's body in which two or more bones meet; the thigh and leg bones meet in your knee. Additionally, the patella, often known as the kneecap, is a tiny bone located at the front of the knee.
Cartilage is the smooth, slick substance that covers the ends of our bones. This relieves pressure on your joints and permits the bones to move against one another without creating friction.
Along with cartilage beneath your kneecap, your knee also has two additional rings of a distinct kind of cartilage called menisci or meniscus, which aid in distributing weight uniformly throughout your knee joint.
Your knee may feel uncomfortable and stiff, move less smoothly than it should, and have thinner cartilage due to osteoarthritis. In addition, the surfaces of the joint grow rougher.
What are the symptoms of osteoarthritis of the knee?
Knee pain:
Patients may have intermittent pain in the knee for more than six months, or they may have pain after engaging in activities that have put stress on the knee, such as long walks, cross-legged sitting, climbing, and descending stairs, hiking, or prolonged car rides, among other activities that may necessitate the knee joint to be bent for an extended amount of time. These activities will only produce discomfort for a short period of time before it goes away in the early stages of the condition; however, the pain will persist considerably longer once the problem reaches a moderate state. Furthermore, even if there is no pressure applied to the knee for a while. For example, while sleeping or resting, that pain will persist. It is even possible that the pain won't go away entirely.
Stiffness and freezing in the knee:
When patients wake up in the morning, they experience these signs, such as a stiffness in the knee, which can cause it to seize up and make movement difficult for about thirty minutes. Every time one’s knee is rested, the stiffness could come back, giving the impression that the joint is immobile and cannot fully flex or extend.
A cracking sound in the knee:
When moving the legs or stretching and bending the joint itself, patients will experience a loud sound that seems like a cracking sound from their knees.
Sensitivity of any area of the knee when pressed:
Any pressure applied to a particular area of the knee can cause pain.
Deformities in the knee:
A knock-knee or bony protrusion may cause patients to perceive that their knee appears larger than usual.
Inflammation:
The inner inflammation will itself cause the knee to swell and possibly feel warm to the touch. If this symptom occurs, it indicates that the patient’s illness has progressed to a somewhat severe level. At this stage, the patient should immediately consult a specialist.

Knee osteoarthritis Diagnosis
Specialists will diagnose the patient’s condition through:
Imaging tests
- An X-ray is usually utilized to diagnose an enlarged tibial tubercle surrounding the knee as well as to find narrowing in the patient's knee joint spaces, as cartilage loss might be discovered by how narrow the space is between the bones in one joint. Medical specialists would typically use X-ray screening, but to rule out other possible causes, a second Magnetic resonance imaging (MRI) scan might be performed to provide a sharper picture of the bone, tissue, and cartilage structure inside the joint. An MRI is crucial when it comes to severe or complex cases.
Laboratory tests
- A blood test helps physicians rule out rheumatoid arthritis and other potential causes of the deterioration.
- Knee scoring: A physician will use a scoring system as an assessment tool to determine the degree of deterioration.

What are the causes of osteoarthritis?
Primary osteoarthritis is brought on by the degeneration of cartilage, a pliable substance that reduces joint friction. Though it generally affects the fingers, thumbs, spine, hips, knees, or large toes, it can occur in any joint.
Older adults are more likely to get osteoarthritis. Overuse of your joints wears down the cartilage, causing pain and swelling. The proteins in the cartilage degrade and water accumulates within. It can begin to peel or develop microscopic tears. In extreme circumstances, it is possible to lose all of the cartilage separating a joint's bones, which causes the bones to rub against one another and increase discomfort when using the joint.
When numerous family members have osteoarthritis, it may indicate that a gene alteration has been passed down from parents to descendants. Seldom do these situations stem from issues with collagen, a strong protein present in your connective tissue.
Let’s dig deep inside the causes, generally, a person's risk of having osteoarthritis is increased by a few variables. These consist of:
- A genetic abnormality associated with one of the genes that produces cartilage can be inherited by certain people. Joint degradation occurs more quickly as a result of this damaged cartilage. Bone osteoarthritis is more common in people with abnormalities of the joints, and bone osteoarthritis of the spine is more common in people with abnormalities of the spine (scoliosis, curvature of the spine, etc.).
- The chance of developing osteoarthritis in the spine, hip, and knee is higher in obese people. Reducing weight or staying at optimal weight can help avoid osteoarthritis in these regions or slow down the disease's course after it has already started.
- Osteoarthritis develops as a result of injuries. For instance, athletes who sustain injuries to their knees may be more likely to develop osteoarthritis in their knees. Furthermore, individuals who have experienced serious injuries to their backs may be more susceptible to developing osteoarthritis in their spine. Osteoarthritis is more likely to develop in a joint in those who have had a broken bone close to it.
- Osteoarthritis is more likely to occur in joints that are overused regularly. Osteoarthritis of the knee, for instance, is more common in those whose employment includes frequent knee bending.
- The risk of developing osteoarthritis is higher in individuals with rheumatoid arthritis, which is the second most common kind of arthritis. Additionally, the likelihood of developing Osteoarthritis is increased by a few uncommon illnesses including iron overload or high growth hormone.
Stem Cell
The body uses stem cells as its basic building blocks, from which every other cell type with specific roles is derived. In the correct circumstances, stem cells can divide in the body or in a lab to produce other cells known as daughter cells.
These daughter cells differentiate into new stem cells or become specialized cells with a more narrowly focused purpose, such as bone, brain, heart, muscle, or blood cells. No other bodily cell possesses the innate capacity to differentiate into new cell types.
There are many advantages to using stem cells in medicine, such as:
- Tissue Regeneration: diseased or injured tissues, including the skin, liver, and heart, can be restored using stem cells. This could completely change how diseases like liver failure, heart disease, and burn injuries are treated.
- Disease Treatment: by restoring damaged tissues or cells, stem cells may additionally be employed to treat illnesses. For instance, they have been used to treat diseases of the neurological system like Parkinson's disease and multiple sclerosis, as well as diseases of the blood, including leukemia as well as other blood disorders.
- Better Understanding of Illness: researchers can better understand the underlying causes of disease and develop novel treatments by using stem cells to examine how diseases arise.
Stem Cells for Knee osteoarthritis
An increasing number of people are turning to stem cell knee injections as a non-surgical way of treating osteoarthritis and persistent knee pain brought on by tears in the tendon, ligament, or cartilage. Using adult stem cells from the patient's own body or from a donor, this type of regenerative medicine aims to reduce inflammation and maybe speed up healing and regeneration. It is possible to get stem cells via aspirating bone marrow from the hip or by using donor cells that are extracted from amniotic fluid and placental tissue. There is no usage of fetal stem cells.
During a first evaluation, the doctor and his specialized orthopedic team will decide if a patient is a good candidate for stem cells. In order to assess the severity of the damage or chronic illness, a diagnostic workup will have to be conducted. Stem cell knee injections are commonly used to treat the following conditions: ligament injuries, osteoarthritis, and cartilage defects
A candidate for stem cells does not have to be a set age, but there are several things to take into account. Adult stem cells from the patient's own body can usually be used to regenerate tissue in patients under 60.
When patients reach 60 years of age, when their body's stem cells begin to decrease, they typically have better outcomes when they combine a healing accelerator, such as platelet-rich plasma (PRP) therapy, with allograft tissue that comes from a different source for regenerated tissue.
How do stem Cells for knees work?
Several researchers have found that the following could happen if stem cells are injected into an arthritic joint:
- Grow into the new cartilage cells required for the joint;
- Reduce the inflammation, which exacerbates arthritis, and release cytokines, which are substances that can either lessen pain or slow down cartilage deterioration.
Related readings:
FAQ:
What are the side effects of injecting Stem cells into the knees?
- Risk of Infection: any injection technique carries a risk of infection. Although this risk is usually minimal, it can be reduced with proper sterilization measures.
- Discomfort and swelling at the injection site: following injections, post-procedure discomfort and swelling are frequent reactions.
- Allergy reactions: While uncommon, there is a little possibility that an allergic reaction to any of the drugs used during the treatment will occur.
- Bleeding and nerve Injury: although rare, injection-based procedures include some risk of bleeding and nerve injury.
- Limited efficacy: some studies suggest that in some cases, it may not be as successful as previously thought in terms of enhancing clinical outcomes and repairing cartilage.
What are the common symptoms of Knee Osteoarthritis?
Osteoarthritis symptoms typically appear gradually and include:
- Aches and pains in the joints, especially when moving
- Soreness from excessive use or extended periods of inactivity
- Stiffness following rest intervals
- Swollen joints
Back


